
ABOUT
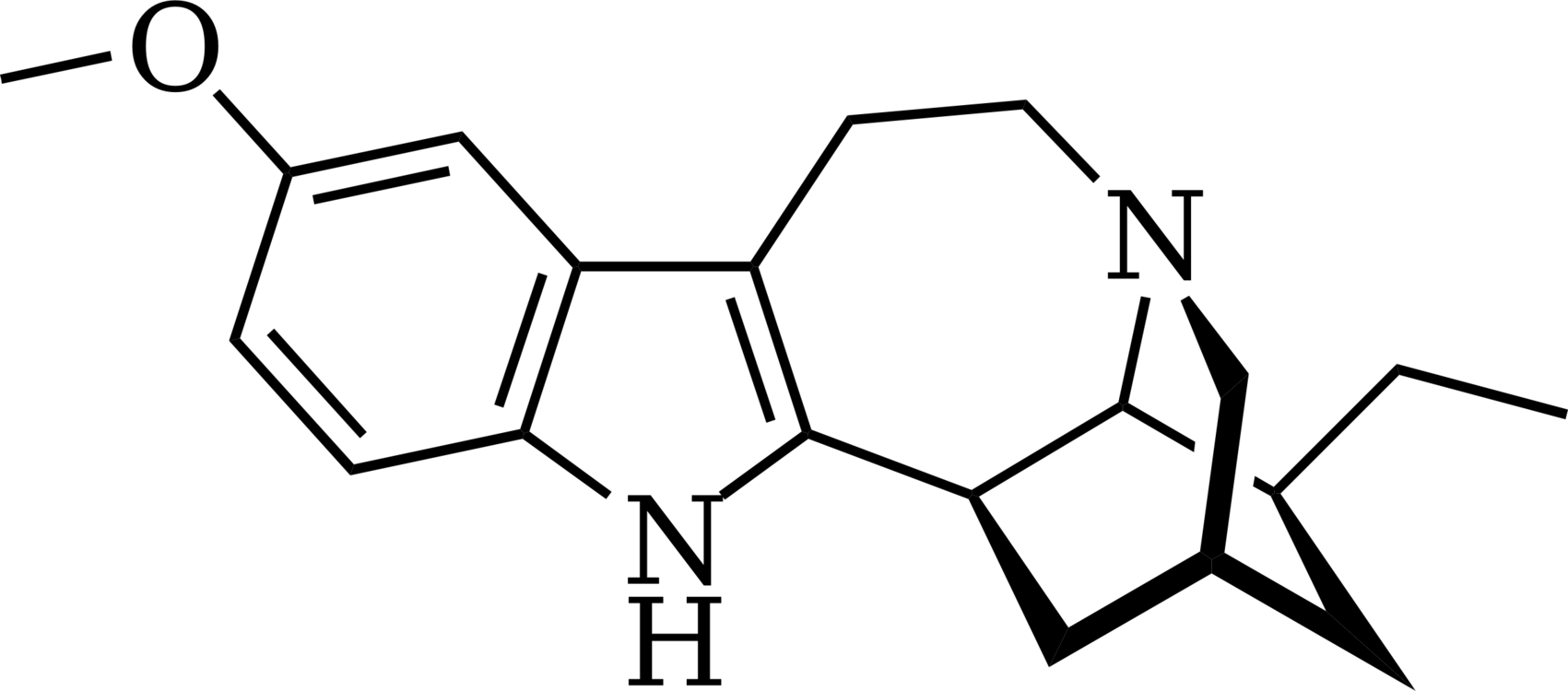
New scientific research provides more evidence that the psychedelic drug ibogaine can help treat opioid withdrawal and cravings. The new findings are reported in the Journal of Psychoactive Drugs.
Malcolm and his colleagues found ibogaine treatment was associated with significant reductions in opioid cravings and withdrawal symptoms. Most of the patients (78%) did not exhibit clinical signs of opioid withdrawal 48 hours after receiving ibogaine. “It seems that ibogaine can interrupt the underlying neurocircuitry of opioid use disorder while delivering a profound psychological experience that reinforces recovery efforts; in our study ibogaine appeared to be able to reduce both the physical signs and symptoms of opioid withdrawal as well as reduce cravings for opioids.” “This means that ibogaine may simultaneously address both physical and psychological aspects of opioid use disorder, whereas other therapeutic agents for opioid use disorders address either physical aspects through continued opioid dependence (methadone, buprenorphine) or psychological aspects of addiction like craving (naltrexone), but do not address both and cannot be used together.”
FACTS
Despite the erroneous labeling as a drug, an “African root that causes severe hallucinations but can be used as a the treatment for heroin addictions””, statistically speaking, many Americans still support legalizing iboga. In fact, iboga is a naturally occurring ethnobotanical and has been used successfully by the traditional African healers for years. There is an opiate epidemic underway, and more potent synthetics like W-18, which is 10,000x more potent than morphine, have been reported just 400 miles north of Eugene, OR for the first time ever.
Can we wait for the next wave of addictive opiates to wash over our green city without a remedy such as iboga on hand? An ethnobotanical that has been scientifically demonstrated to make opiate withdrawals virtually vanish. South Africa thinks so, and just medicalized the plant. Vermont is also considering similar measures. From the ethnobotanical angle, the iboga plant could be grown by anyone, it’s healing properties utilized to alleviate human suffering. However this would leave any would be grower of this plant to face stiff penalties, harsh prison sentences, and even the loss of parental rights. Does that sound a little bit like cannabis prohibition once did?
In a time of urgency, as the Afghanistan government has eliminated it’s poppy eradication program leading some farmers to yield up to four times more poppies this year, a marked increase in opiate availability may too come to pass. This, in addition to the synthetic opiate W-18 entering the market place. Without the availability of iboga and other ethnobotanicals for addiction treatment available, our best harm reduction practices are to build more treatment centers for millions of dollars. These very centers which are coming increasingly under-fire from the general community and in Behavioral Town Hall Meetings, and in broad terms, increase supplies of methadone (another form of opiate).
In short, opiates are expensive, and scientifically unsuperior when compared with iboga, and other ethnobotanicals. As a modern philosopher and spiritual teacher once wrote, “Hope and Fear cannot change the season”. The rains have come, the harvest is in, and the arm of “supply side” enforcement has eased it’s prohibitive grip, potentially, releasing a new tide of opiates the American population. A population, which seems to maintain a robustly healthy appetite for them. Our community is well-served when well-informed.
And finally, the iboga plant, which was declared a National Heritage in Gabon in 2000, is currently considered a threatened species. “Although people aren’t permitted to collect the plant without authorization, from the government, there is nevertheless excessive harvesting”. Reports are the plant could disappear from the public domain in less than 5 years.



SCIENTIFIC EVIDENCE / MEDICINAL EFFICACY
- A single ibogaine treatment reduced opioid withdrawal symptoms and achieved opioid cessation or sustained reduced use independent individuals as measured over 12 months. Ibogaine’s legal availability in New Zealand may offer improved outcomes where legislation supports treatment providers to work closely with other health professionals. – Read More
- A four-day treatment with ibogaine was successful in achieving long-term remission of a previously treatment-refractory patient with severe Opioid Use Disorder. the case of a 37-year-old female with a 19-year history of severe OUD achieving an ongoing 18-month period of abstinence following a four-day ibogaine treatment. Her previous longest period of continuous abstinence from opioids was two months while on methadone. – Read More
- Results suggest that the use of ibogaine supervised by a physician and accompanied by psychotherapy can facilitate prolonged periods of abstinence, without the occurrence of fatalities or complications. These results suggest that ibogaine can be a safe and effective treatment for dependence on a stimulant and other non-opiate drugs. – Read More
- Behavioral pharmacologic studies in animal models provided evidence that ibogaine could blunt self-administration of not only opiates but cocaine, amphetamines. – Read More
